Understanding 12-Week Genetic Testing After IVF
IVF has the potential to bring about pregnancy, and with it, a whole range of emotions: excitement, hope, and natural worries about the health of the baby. The early discovery of chromosomal and sex-linked disorders might, for instance, give the couples undergoing assisted reproduction a great deal of comfort.
Genetic testing has gradually evolved into a significant factor in prenatal care, detecting possible risks at an early stage. The 12-week genetic testing, which is also known as Non-Invasive Prenatal Testing (NIPT), is one of the most successful alternatives in this regard; it has been acknowledged as very accurate and safe.
We are going to clarify the process of 12-week genetic testing, the reasons for its frequent recommendation after IVF, its functioning, and the results you may receive in this guide.
Are you wondering what makes 10-week genetic testing so vital in your pregnancy?
Let’s delve into how this simple blood test can give you peace of mind and early insight into your baby’s health.
What Is 12-Week Genetic Testing?
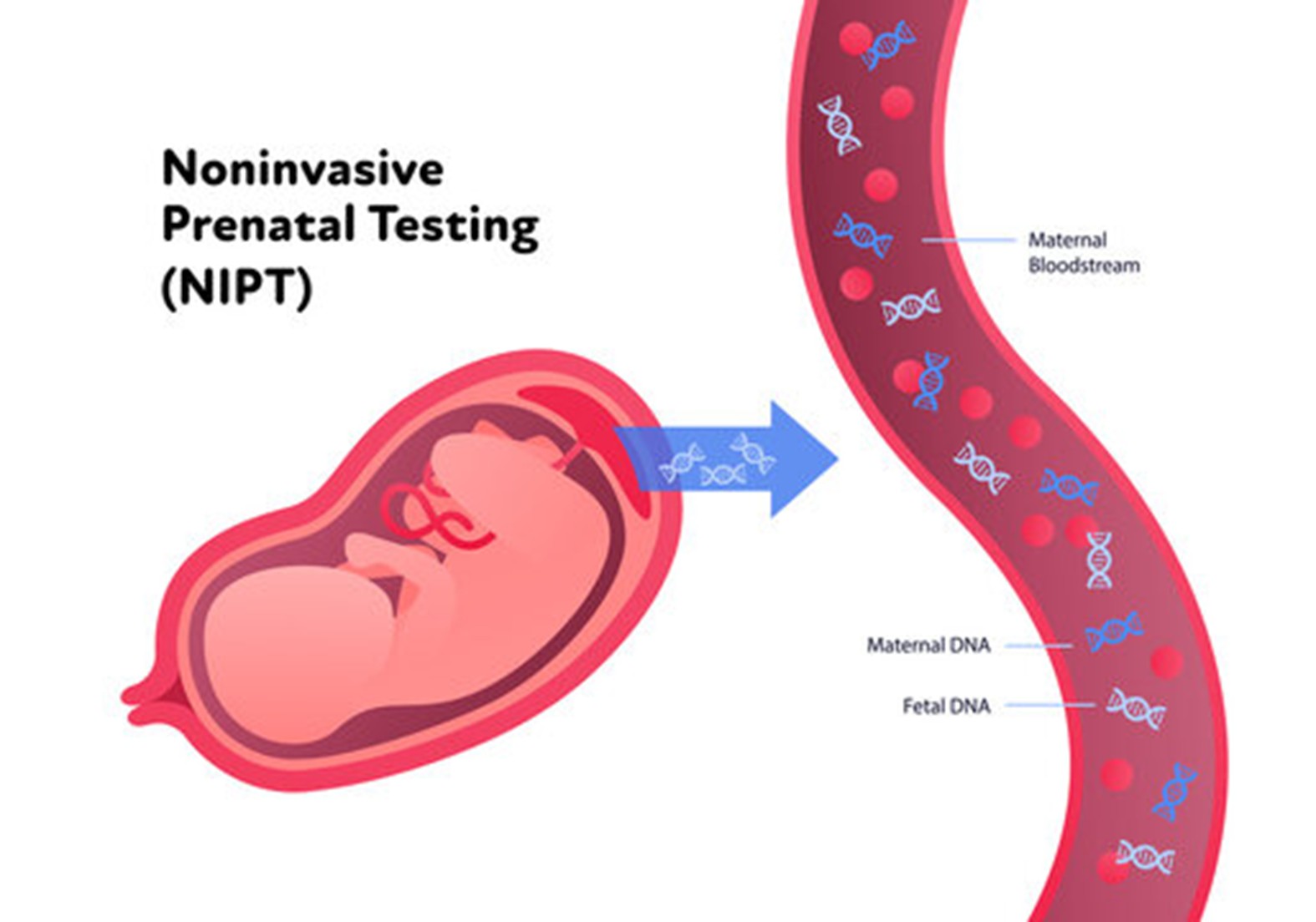
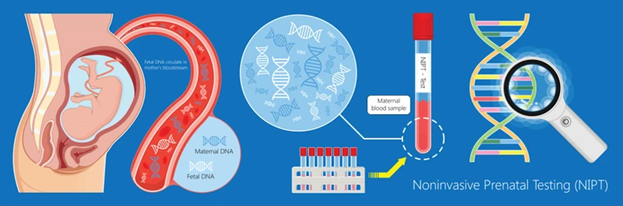
12-week genetic testing is a non-invasive blood test (NIPT) usually performed around the 12th week of pregnancy. It examines a small fraction of fetal DNA present in the mother’s blood to assess the risk of certain chromosomal disorders, including:
Trisomy 21 (Down Syndrome)
Trisomy 18 (Edwards Syndrome)
Trisomy 13 (Patau Syndrome)
Unlike invasive procedures such as amniocentesis or chorionic villus sampling (CVS), NIPT poses no risk to the mother or baby, making it a safe option for IVF pregnancies.
Why 12-Week Genetic Testing Matters After IVF
Implantation embryos through IVF generally come with early genetic screening as a priority. The 12-week NIPT, however, is worth the mention for the following reasons:
Early Detection of Chromosomal Conditions
NIPT in the first trimester uncovers major genetic issues and so, gives the parents more time to be ready and organized.
Safe and Non-Invasive
The only thing the test requires is a blood sample from the mother which makes it absolutely safe for both mother and baby—especially given that IVF pregnancies are often viewed as high-risk.
Highly Accurate Results
NIPT gives more than 99% accuracy for Down syndrome and very high detection rates for other common chromosomal abnormalities; thus, it is one of the most reliable prenatal screening tools.
Emotional Reassurance
The results showing low risk help the parents to relieve their stress, and thus, they will be able to enjoy their pregnancy journey with certainty.
Suitable for All IVF Pregnancies
NIPT can be offered to all types of IVF pregnancies, be it ICSI, fresh, or frozen embryo transfer, irrespective of the maternal age or history.
Curious about the process behind 10-week genetic testing?
Let’s explore the steps involved and how the test works to analyze fetal DNA for key genetic conditions
How Does 12-Week Genetic Testing Work?
Here’s a step-by-step look at the testing process:
Blood Sample Collection
At the prenatal visit, a blood sample is taken from the mother. This sample contains both maternal and fetal DNA, with the fetal portion isolated for testing.
DNA Analysis
The lab examines the fetal DNA for chromosomal abnormalities, including extra copies of chromosomes 21, 18, and 13. The test can also determine the baby’s gender, though this is secondary to its main purpose.
Results
Results are typically available within 7–10 working days and are categorized as:
- Low Risk: Very low probability of the screened conditions
- High Risk: Increased likelihood, but not a definitive diagnosis
Next Steps
If results indicate high risk, your doctor may recommend confirmatory tests such as CVS or amniocentesis along with genetic counseling. Low-risk results usually do not require additional genetic testing, though routine prenatal care continues.
Want to know exactly what this test can screen for?
Let’s discuss the common chromosomal conditions it can help detect and what that means for your pregnancy
What Conditions Can 12-Week Genetic Testing Detect?
The test primarily screens for:
DNA Analysis
The lab examines the fetal DNA for chromosomal abnormalities, including extra copies of chromosomes 21, 18, and 13. The test can also determine the baby’s gender, though this is secondary to its main purpose.
Results
Results are typically available within 7–10 working days and are categorized as:
- Low Risk: Very low probability of the screened conditions
- High Risk: Increased likelihood, but not a definitive diagnosis
Next Steps
If results indicate high risk, your doctor may recommend confirmatory tests such as CVS or amniocentesis along with genetic counseling. Low-risk results usually do not require additional genetic testing, though routine prenatal care continues.
Blood Sample Collection
At the prenatal visit, a blood sample is taken from the mother. This sample contains both maternal and fetal DNA, with the fetal portion isolated for testing.
Trisomy 18 (Edwards Syndrome):
Associated with severe developmental challenges
Trisomy 13 (Patau Syndrome):
Rare but serious condition causing major health complications
Sex Chromosome Abnormalities (Optional)
Can detect conditions like Turner or Klinefelter syndrome
Wondering how 10-week genetic testing can benefit you and your pregnancy?
Let’s dive into the key advantages and why many parents choose this non-invasive screening option.
Benefits of 12-Week Genetic Testing for IVF Pregnancies
Provides early reassurance in the first trimester
Exceptional accuracy for common chromosomal conditions
No risk of miscarriage
Helps in informed medical and personal decision-making
Enables timely specialist consultation if needed
Curious if there are any potential drawbacks to 10-week genetic testing?
Let’s explore the limitations and what you should consider before deciding if it’s right for you.
Are There Any Limitations?
Screening, Not Diagnostic: High-risk results require confirmatory tests
Limited Scope: Does not detect all genetic disorders or structural birth defects
Cost Considerations: Insurance coverage varies; some out-of-pocket expense may apply
Discussing these factors with your fertility specialist can help you decide if NIPT is right for your pregnancy.
Connect with your doctor now and discuss the benefits of 10-week genetic testing to gain valuable insights into your baby’s health early on.
Conclusion
For couples conceiving through IVF, 12-week genetic testing provides a safe, accurate, and early assessment of your baby’s genetic health. While it cannot offer a definitive diagnosis, it is a crucial tool for early risk evaluation, guiding further care and informed decisions.
If you’re considering genetic testing after IVF, speak with your fertility specialist or obstetrician to see how NIPT fits into your personalized prenatal care plan.
Frequently Asked Questions
What is 12-week genetic testing after IVF?
A non-invasive blood test (NIPT) that screens for common chromosomal abnormalities using fetal DNA from the mother’s blood.
Is NIPT safe for IVF pregnancies?
Yes, it is completely safe and involves no risk to mother or baby.
Which conditions does it screen for?
Primarily Down syndrome, Trisomy 18, Trisomy 13, and optional sex chromosome abnormalities.
How accurate is the test?
Over 99% accurate for Down syndrome and highly sensitive for other conditions.
When will I receive results?
Typically within 7–10 working days.