Ovarian hyperstimulation syndrome (OHSS) is a side effect of fertility medication that involves using pharmacological substances to promote ovarian stimulation to increase the number of oocytes and thus the number of embryos accessible during assisted reproductive technology (ART).
The ovarian response exceeds that goal in a small percentage of female patients undergoing IVF treatment in Ahmedabad, resulting in clinical diseases with distinct aetiology. The most severe side-effect of ovulation induction is ovarian hyperstimulation syndrome (OHSS). It causes a wide range of symptoms.
In women undergoing assisted reproduction, it manifests as an increased reaction to ovulation induction. The risk of OHSS differs depending on the type of fertility approach used, with therapies involving higher levels of ovarian stimulation having a higher risk.
Now, let’s know,
Classification of OHSS
Clinical criteria are used to make the diagnosis. Fertility specialists use clinical symptoms, ultrasound findings, and laboratory markers to classify OHSS into different phases and grades. So, having a distribution based on symptoms is critical.
In a fertility clinic in Ahmedabad, mild and moderate ovarian hyperstimulation syndrome can be treated promptly in an outpatient setting. The specialist can hospitalize patients with severe OHSS to an ICU.
Fortunately, severe OHSS is quite rare when using advanced treatment procedures. So, early detection and timely evaluation and treatment of patients with moderate or severe OHSS are fundamental concepts of OHSS management.
Types of Ovarian Hyperstimulation Syndrome
Early: After 5 to 7 days of taking the hCG trigger shot.
Late: After detection of pregnancy, it is observed.
Now, let’s know,
Sign and Symptoms of OHSS
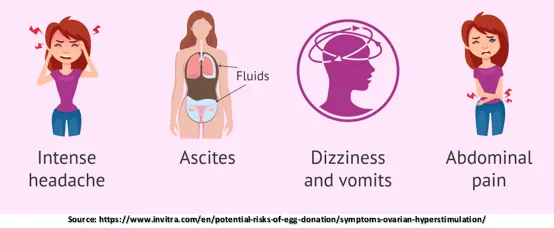
OHSS signs and symptoms are divided into three categories based on their severity:
Mild OHSS
- Abdominal bloating
- Swelling in the abdomen
- Nausea
- Increase in waistline with minor discomfort
Moderate OHSS
- Abdominal discomfort
- Nausea and vomiting
- Headache
- Ultrasound reveals fluid (ascites) build-up in the abdomen
- Decreased urination
Severe OHSS
- Nausea and severe abdominal discomfort.
- Dehydration and extreme thirst.
- Decreased urination with dark-colored urine.
- Breathing problems.
- Swelling in legs due to clotting.
- Abdomen enlargement.
- Sudden weight gain over 24 hours.
Now, let’s discuss,
Diagnosis of OHSS
Following the trigger shot to encourage final follicular maturation before oocyte retrieval, the average patient has stomach distension and discomfort.
There may have been a previous record of an extreme ovarian stimulation response, but this does not rule out an analysis of OHSS.
Patients are divided into two categories based on when they present after receiving the trigger injection:
Diagnosis of early and late OHSS
These women’s ovarian responses may be ordinary at first. Early OHSS occurs within seven days of receiving the hCG shot. It is frequently linked with an overactive ovarian response.
Endogenous hCG produced from early pregnancy is usually the cause of late OHSS. It appears within or more than ten days after the hCG shot. Late OHSS is more severe and lasts longer than the earlier variant.
To diagnose OHSS, the doctor will take the below steps:
Take a complete medical history of a patient suspected of having OHSS.
History
- Relative to a trigger, the time when symptoms first appear.
- Trigger-relieving medication.
- Number of follicles on the final monitoring scan.
- The total number of eggs harvested.
- Was there placement of embryos, and how many were placed?
- Diagnosis of PCOS?
Symptoms
- Bloating in the abdomen.
- Need of analgesia due to abdominal pain.
- Vomiting.
- Nausea.
- Unable to lie flat or speak in whole phrases.
- Shortness of breath.
- Reduced urine production.
- Swelling in the legs.
- Swelling of the vulval cavity.
- Thrombosis and other comorbidities.
Examination of women with suspected OHSS
General Exam:
Examining dehydration and edema (vulval, pedal, and sacral). Recording the heart rate, blood pressure, breathing rate, and weight.
Abdominal Exam:
Examine ascites, peritonism, palpable mass, and girth.
Respiratory Exam:
Determine whether there is pneumonia, pleural effusion, or pulmonary edema.
Investigations:
- Complete blood count
- CRP count
- Haematocrit
- Urea and electrolytes
- LFT
- Coagulation profile
- Serum osmolality
- hCG (to discover the outcome of treatment) if proper
- Ultrasound scan: size of ovaries, pelvic and abdominal fluid.
- If torsion is suspected, an ovarian Doppler is considered.
Other tests may include:
- Chest X-ray
- D-dimers
- ECG
- CTPA
Steps Taken for Prevention of OHSS
- Identifying a high-risk patient is the most important step in preventing OHSS.
- Several epidemiologic, hormonal, and ultrasound findings of individuals who are most likely to develop OHSS should be kept in mind by all clinicians.
- An average patient is young, with a slim physique and PCOD-like hormonal composition indicates ultrasound.
- If a patient has higher E2 levels during ovarian stimulation and many small, intermediate follicles are visible on ultrasound, the doctor should be on high alert.
- When a patient is at higher risk, the doctor mostly avoids an hCG shot or replaces it with a GnRH shot.
Management of OHSS
- Because the cause of OHSS is unknown, treatment is mainly based on trial and error.
- The first-line treatment for mild to moderate ovarian hyperstimulation syndrome is bed rest, plenty of liquids, and painkillers.
- The signs of intravascular volume reduction and hyponatremia can be managed with a balanced salt solution.
- Massive Ascites and hemoconcentration indicate that OHSS has progressed to a severe stage, necessitating hospitalization and IV.
Consult an experienced IVF doctor in Ahmedabad to receive safe and result-oriented assisted reproduction treatment to achieve a successful pregnancy.