
Fertility Tests and Assessments in Ahmedabad
Getting pregnant may seem easy, but conceiving a child can often be challenging. Many bodily functions and processes must be in good working order in both men and women. Infertility occurs when a couple cannot conceive even after natural unprotected sex.
Your regular gynecologist will do basic tests. They may recommend you to a fertility doctor for further in-depth analysis. Through testing, your doctor can discover the cause that is hindering your pregnancy.
At Nisha IVF Centre, one of the top-rated IVF Centre in Ahmedabad, our primary focus is to fulfill your dream of parenthood by implementing the most suitable fertility treatment. Our highly experienced and proficient fertility specialist will evaluate you and your partner and perform specific tests. Those will help determine the underlying condition that is obstructing conception.
Now, let’s know which fertility tests and assessments our expert gynecologists, fertility specialists, and IVF doctor in Ahmedabad perform to determine the root cause of your infertility.
Your fertility expert will perform specific tests if you haven’t got pregnant even after trying for six months. Your doctor may check your hormone levels, your reproductive organs such as ovaries, fallopian tubes, and uterus, and your partner’s sperm using different methods.
1. Evaluation of the Uterus
There are various tests to examine your uterus.
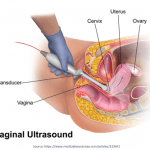
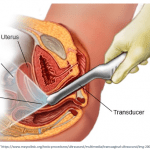
A. Vaginal Ultrasound:
A tampon-like probe is inserted into the vagina to perform a vaginal ultrasound. The probe transmits sound waves to a screen, displaying an enhanced image of uterus walls, lining, and ovaries.
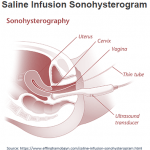
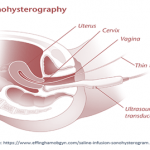
B. Sonohysterogram (Saline Infusion Sonogram):
It is a special type of vaginal ultrasound. It involves placing a small amount of sterile fluid in your uterus through a tiny plastic tube. It allows your doctor to inspect the shape of the uterus’s cavity.
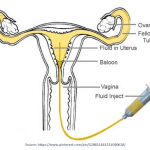
C. Hysterosalpingogram (HSG):
It gives information about the fallopian tubes and the uterus. It involves placing a small amount of a special radio-opaque dye into your uterus through the cervix. After the dye injection, an X-ray is taken to show the dye’s path through the uterus and fallopian tubes. This test helps view the cavity’s shape and check whether the fallopian tubes are open.
D. Hysteroscopy:
It involves using a small telescope (hysteroscope) attached to a camera to look inside the uterus to diagnose and treat specific problems. It is passed through the cervix into the uterus under anaesthesia. It gives the most accurate information about the uterus cavity.
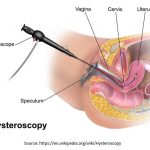
Types of Hysteroscopy:
1. Diagnostic hysteroscopy:
It helps diagnose infirmities inside the uterus.
2. Operative hysteroscopy:
It helps remove abnormal tissue that can cause fertility or bleeding problems.
What can Hysteroscopy be used to diagnose and treat?
- Endometrial polyps are small growths on the uterus lining. They may affect fertility and can cause abnormal bleeding.
- Uterine fibroids are noncancerous growths on the uterus wall. They can cause heavy bleeding and problems in conceiving if present inside the uterus.
- Scar tissue (adhesions) inside the uterus can be removed using hysteroscopy.
- The uterine septum is a tissue that divides the uterus in half. It is a uterine abnormality that some women are born with and can cause miscarriages.
What are the Risks of Hysteroscopy?
Severe hysteroscopy complications are extremely rare. Like after any procedure, you could get few side-effects with hysteroscopy like:
- Infection
- Bleeding
- Pelvic inflammatory disease
- Tearing of the uterus (rare) or damage to the cervix
- Complications from fluid or gas used to expand the uterus
In case of heavy bleeding, you should seek immediate medical care.
2. Diagnostic Testing for Female Infertility
Being evaluated earlier is better after six months of unprotected sex for women who are older than age 35 or who have:
- Medical history of irregular menstrual cycles (about 35 days apart or no menses at all)
- Known or suspected infirmities with the uterus, tubes, or other issues in the abdominal cavity (like endometriosis or adhesions)
The following tests are some of the female infertility tests:
A. Transvaginal Ultrasonography:
It involves placing an ultrasound probe in the vagina. It allows the doctor to examine the uterus and ovaries for abnormalities such as fibroids, polyps, and ovarian cysts.
B. Ovarian Reserve Testing:
It helps determine whether the woman is producing an egg or eggs of good quality. They also test whether the ovaries are correctly responding to the hormonal signals from the brain.
The following are the most common tests to evaluate ovarian reserve:
1. Blood test for Anti-Mullerian hormone (AMH), Follicle-stimulating hormone (FSH), Oestradiol, and Inhibin-B
2. Transvaginal ultrasound to perform an antral follicle count, the number of follicles or egg sacs viewed during the initial menstrual cycle.
The ovarian reserve testing is relevant for females at a higher risk of reduced ovarian reserve, such as women who:
- are above 35 years
- have a family history of early menopause
- have a single ovary
- have a medical history of ovarian surgery, chemotherapy, or pelvic radiation therapy
- have unexplained infertility
- have shown an inadequate response to ovarian gonadotropin stimulation
3. Other Blood Tests:
- Thyroid-stimulating hormone (TSH) and Prolactin levels are helpful to identify thyroid disorders and hyperprolactinemia. These may cause problems with fertility, menstrual inconsistencies, and repeated miscarriages.
- In women at risk of increasing hirsutism, blood tests for dehydroepiandrosterone sulfate (DHEAS), 17-α hydroxyprogesterone, and total testosterone may be ordered by your clinician.
- A blood progesterone level drawn in the second half of the menstrual cycle can test whether ovulation has occurred.
4. Urinary Luteinizing Hormone (LH):
Over-the-counter “ovulation predictor kits” may detect the presence of LH in the urine. It can detect a rise in this hormone that occurs one to two days before ovulation. In contrast to blood progesterone levels, urinary LH tests can predict ovulation before it happens.
C. Sonohysterography:
It involves using transvaginal ultrasound after filling the uterus with saline. It improves the detection of intrauterine problems such as endometrial polyps and fibroids compared with using transvaginal ultrasonography alone. Your doctor may perform hysteroscopy after detection of an abnormality. They do this test in place of HSG.
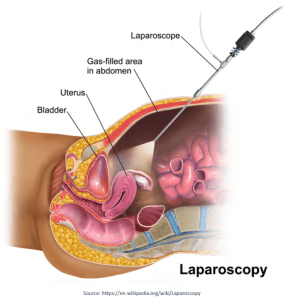
D. Laparoscopy:
It is a minimally invasive procedure that involves the insertion of a lighted telescope-like instrument (laparoscope) through the abdomen’s wall into the pelvic cavity. It helps evaluate the pelvic cavity for endometriosis, pelvic adhesions, and other abnormalities.
For best results, the infertility evaluation should be individualized based on each woman’s specific circumstances.
3. Diagnostic Testing for Male Infertility
When a couple has problems in conceiving, there’s a 50-50 chance that the male faces difficulties in achieving pregnancy.
He could:
- Produce fewer sperms to fertilize an egg.
- Make sperms that are abnormally shaped or have low motility.
- Have a blockage in the reproductive tract that prevents the sperm’s entry.
If you have a fertility problem, your doctor will record a complete medical history and perform a physical exam. They may order several tests to determine the cause of your infertility.
A. Semen Analysis
Semen is the fluid released when a male has an orgasm. The semen comprises the sperm in fluids that should nourish and preserve it. Your doctor will tell you to give a semen sample. The semen analysis presents information about the quantity and quality of the semen and sperm.
Some of the aspects that are measured include:
- The volume of semen produced
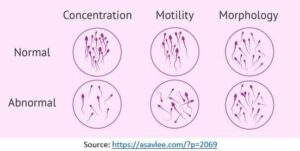
- Total number of sperms in the semen sample
- Quantity of sperms in each milliliter of semen (concentration)
- Percentage of sperm that are moving (motility)
- The shape of sperms (morphology)
The analysis can also reveal any infection in the male reproductive tract. Within an hour of collection, the semen sample must be checked. Before supplying the semen sample, you can be asked to avoid releasing sperm (ejaculate) for 2 to 5 days.
B. Hormone Levels and Reproduction
Hormones are essential chemicals that regulate the production of sperm. They also affect your desire for and ability to have sex. These hormones can cause problems with sperm production and intercourse if they are too high or too low.
Follicle-stimulating hormone (FSH) and testosterone are two essential hormones for reproduction. Your doctor might need a blood test to find whether you have the correct amount of these hormones. Other hormonal levels, such as Luteinizing hormone (LH), Oestradiol, and Prolactin, may be checked if necessary.
C. Other tests
If semen analysis results aren’t normal, you may require more tests. These tests will show:
- If sperms are alive in the semen sample (“Vital Staining” test).
- If antibodies are attached to the sperm, making it difficult for the sperm to move swiftly (“Anti-sperm Antibody” test).
- If you’re suffering from an infection or inflammation that is affecting the semen quality (“Peroxidase Staining” and “Semen Culture”).
D. Additional tests
If you’ve had the above tests, but the infertility issues are still not revealed, then you may need additional tests. These tests will determine:
- If the sperm’s outer layer is broken or intact (“Hypo-osmotic Swelling” test)
- If your sperms are moving the way they should (“Computer-assisted Semen Analysis”)
- If too many of your sperms have broken or fragile DNA (“Sperm DNA Testing”)
- If your sperm have the exact number of chromosomes (Sperm Aneuploidy testing)
- If you have a chromosomal defect (Chromosome analysis and Y-chromosome deletion testing)
- If sperms are absent (Check if the sperm tubes are intact or perform a testicles biopsy)
No semen analysis can completely predict fertility. Other than a semen test, not all tests discussed are relevant for every couple.
If you’re facing problems in achieving pregnancy, book an appointment with our fertility experts to seek the most effective treatment.
