Navigating life after a hysterectomy can be a transformative journey. However, for many women, the challenges of bowel endometriosis persist. Are you grappling with bowel endometriosis after hysterectomy? You’re not alone. Studies show that around 12-32% of women with endometriosis experience bowel involvement post-hysterectomy.
Managing endometriosis of the bowel after hysterectomy requires a tailored approach. Dr. Nisarg Patel advises comprehensive evaluation to determine the condition’s extent. Timely and accurate diagnosis with expert intervention can improve bowel endometriosis symptoms after hysterectomy.
Dr. Nisarg Patel and his team at Nisha IVF, renowned as the best IVF centre in Ahmedabad, specialize in providing personalized care. Dr. Patel is adept at addressing the unique needs of women in this post-operative phase. He ensures your concerns are understood and met with the most effective strategies.
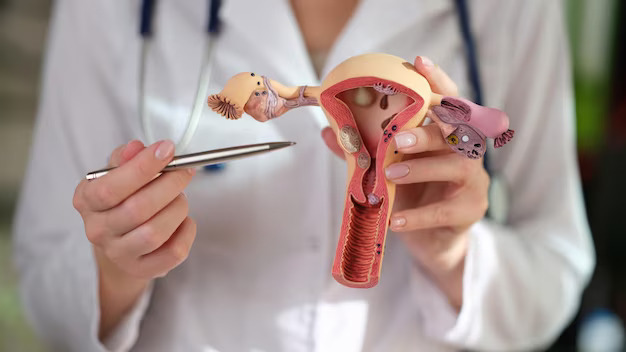
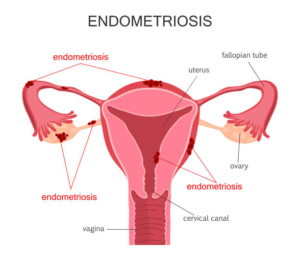
Overview of Bowel Endometriosis after Hysterectomy
This condition occurs when endometrial tissue, found in the uterus, grows on the bowel or adjacent areas after a hysterectomy. It can lead to various symptoms including:
- abdominal pain
- bloating
- changes in bowel habits
Uterus removal during a hysterectomy doesn’t guarantee the complete eradication of endometriosis. Sometimes, the endometrial tissue persists or develops on nearby organs like the bowel. This can result in the recurrence of symptoms, impacting the patient’s quality of life.
Dr. Nisarg Patel, widely known as the best IVF doctor in Ahmedabad, ensures patients receive the most effective treatment tailored to their unique situation.
Wondering if those post-surgery bowel issues are a common occurrence? Let’s dive into the commonality and what to expect.
Is it Normal to have Bowel Issues after Hysterectomy?
Experiencing bowel issues after a hysterectomy is not uncommon. Many women may encounter changes in bowel habits during the post-surgery phase. It is considered a normal part of the recovery process. Yet, understanding the reasons behind these changes is crucial.
The proximity of the uterus to the bowel and the intricate network of nerves in the pelvic region can contribute to alterations in bowel function.
Studies suggest that up to 30% of women may experience bowel dysfunction post-hysterectomy. It manifests as constipation, diarrhoea, or changes in bowel frequency. It is important to stay informed and communicate openly with your healthcare provider. They ensure personalized care and support tailored to your unique needs.
For personalized, long-term care, book an appointment with Dr. Nisarg Patel at Nisha IVF Hospital in Ahmedabad.
Curious about the duration of post-hysterectomy bowel problems? Let’s unravel the timeline and ease any concerns you may have.
How Long do Bowel Issues Last after Hysterectomy?
Experiencing bowel issues after a hysterectomy is common, but the duration varies. Typically, the initial weeks post-surgery may bring temporary disruptions. This includes issues such as constipation or irregular bowel movements. These issues often stem from factors like:
- anaesthesia
- reduced physical activity
- dietary changes during recovery
It is normal for your bowel habits to gradually normalize as your body heals. However, persistent bowel issues beyond the initial recovery phase warrant attention.
“If discomfort or irregularities persist for an extended period, it is crucial to consult a healthcare provider,” advises Dr. Nisarg Patel. “They can assess your specific situation and rule out any underlying concerns. Based on the diagnosis, they can recommend appropriate treatment to ensure your comfort and well-being.”
Let’s know the factors contributing to endometriosis of the bowel after hysterectomy.
What Causes Bowel Endometriosis After Hysterectomy?
1. Residual Endometrial Tissue:
- Some endometrial tissue may be left behind after a hysterectomy.
- Residual tissue can lead to the development of bowel endometriosis.
2. Spread During Surgery:
- Endometrial cells might spread to the bowel during hysterectomy.
3. Pre-existing Endometriosis:
- If the patient had endometriosis before the hysterectomy, there is a risk of it affecting the bowel post-surgery.
4. Hormonal Factors:
- Hormonal fluctuations post-hysterectomy can stimulate residual endometrial tissue. It can trigger bowel endometriosis.
Understanding these causes is crucial for managing bowel endometriosis after hysterectomy.
If you are experiencing concerns, consult Dr. Nisarg Patel, a seasoned fertility expert, for personalized guidance and support.
Discovering effective strategies to manage endometriosis of the bowel after hysterectomy? Your roadmap to recovery starts here.
Treatments for Bowel Endometriosis After Hysterectomy
Dealing with bowel endometriosis post-hysterectomy requires tailored treatments for optimal recovery. Your path to relief involves a combination of approaches, personalized to your needs.
1. Medication Management:
Ease discomfort with targeted medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help control pain. Your doctor may prescribe hormonal therapies like birth control pills or GnRH agonists. These can help regulate hormone levels, curbing endometrial tissue growth.
2. Lifestyle Modifications:
Simple changes can make a significant impact. Regular exercise promotes overall well-being. It also aids in managing pain and reducing inflammation. Dietary adjustments, such as incorporating anti-inflammatory foods, may complement your treatment plan.
3. Surgical Interventions:
In some cases, surgical options might be recommended. Advanced techniques, like laparoscopic excision surgery, help remove endometrial tissue. This procedure also focuses on preserving surrounding organs.
Schedule a consultation with Dr. Nisarg Patel for personalized surgical solutions.
4. Ongoing Monitoring and Support:
Regular check-ups and open communication with your healthcare team are crucial. Address concerns promptly and keep them informed of any changes in symptoms.
Dr. Nisarg Patel and his team at Nisha IVF Hospital are here to support you on your journey to relief. Remember, your treatment plan is as unique as you are. With a proactive and collaborative approach, you can manage bowel endometriosis after hysterectomy.
Let’s discuss the potential long-term implications of bowel endometriosis after hysterectomy. Gain insights into proactive measures and ongoing care to promote your well-being.
Long-Term Problems with Endometriosis After Hysterectomy

1. Pelvic Pain Persistence:
- Pelvic discomfort may continue post-hysterectomy due to persistent endometriosis.
- Consult with your healthcare provider for effective pain management strategies.
2. Adhesion Challenges:
- Adhesions, or scar tissue formation, can occur after surgery.
- Discuss concerns about adhesions with your doctor for potential solutions.
3. Hormonal Shifts:
- Hormonal imbalances may persist despite the removal of the uterus.
- Regular follow-ups with your healthcare provider can help manage hormonal fluctuations.
4. Gastrointestinal Issues:
- Bowel endometriosis can lead to ongoing gastrointestinal problems.
- Report any digestive concerns to your doctor for tailored interventions.
5. Emotional Well-being:
- Emotional challenges may surface due to the persistent nature of endometriosis.
- Seek support from healthcare professionals or support groups to address emotional well-being.
Stay in regular communication with your healthcare team. It ensures a proactive approach to managing long-term challenges associated with endometriosis post-hysterectomy.
For comprehensive care and long-term management, schedule a consultation with Dr. Nisarg Patel at Nisha IVF Hospital in Ahmedabad.
Outlook
In conclusion, the outlook for bowel endometriosis after hysterectomy is promising for many. Proactive and individualized care plays a pivotal role. Stay informed, communicate openly with your healthcare provider, and prioritize your post-surgery well-being.
Remember, you are not alone in this journey. Dr. Nisarg Patel at Nisha IVF Hospital is here to guide you every step of the way. Connect with Dr. Nisarg Patel to discuss your case and develop a personalized care plan.
Find answers to common queries on bowel endometriosis after hysterectomy. Empower yourself with knowledge for a smoother recovery journey.
Frequently Asked Questions:
1. Can bowel endometriosis recur after hysterectomy?
Yes, while hysterectomy can reduce symptoms, there’s a chance of bowel endometriosis recurrence. Regular follow-ups with your healthcare provider can help address any signs of recurrence.
2. How long does it take to recover from bowel endometriosis after hysterectomy?
Recovery time varies. Many women experience improvement in symptoms within a few weeks post-hysterectomy. Dr. Nisarg Patel advises personalized care and follow-ups. It ensures a smooth recovery tailored to your individual needs.
3. What lifestyle changes can help manage bowel endometriosis after hysterectomy?
Adopting a healthy lifestyle is crucial. Dr. Nisarg Patel recommends a balanced diet, regular exercise, and stress management. These factors contribute to well-being. It can impact the management of bowel endometriosis post-hysterectomy.
4. Are there alternative treatments for bowel endometriosis after hysterectomy?
Alternative treatments such as hormonal therapy can be considered. Dr. Nisarg Patel discusses individualized options based on your health profile and preferences.
5. Can I conceive after a hysterectomy for bowel endometriosis?
Hysterectomy involves the removal of the uterus, impacting natural conception. Dr. Nisarg Patel specializes in IVF treatments. He can discuss assisted reproductive options tailored to your circumstances and fertility goals.